AUTISM
SPECTRUM DISORDER
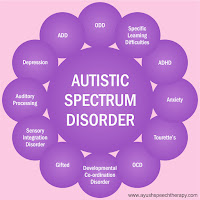
Autism spectrum disorder (ASD) is a developmental disorder characterized
by symptoms appearing in early childhood and impairing day-to-day life
function. These symptoms include qualitative impairments in
social/communication interaction and repetitive and restricted behaviors,
according to the Diagnostic and Statistics Manual of Mental Disorders. Under the umbrella of ASD, a patient’s symptoms will fall on
a continuum, with some showing mild symptoms and others, more severe. A
diagnosis under the general diagnostic category of ASD is relatively new. Prior
to the publication of DSM-5, there were five ASDs, each of which had a unique
diagnosis: classic autism, pervasive developmental disorder (PDD), Asperger’s
disorder, Rett’s syndrome, and childhood disintegrative disorder. With the
exception of Rett’s syndrome, these disorders are now subsumed into the diagnosis
of ASD. Rett’s syndrome is now its own entity and is no longer a part of the
autism spectrum.
ASD is thought to have an early onset, with symptoms appearing
before 24 months of age in most cases. Although a definitive diagnosis of
autism is not generally made until the age of 3 years or later (Mandell et al.,
2005), there are a growing number of reports of stable diagnoses following
identification as young as 2 years (Chawarska et al., 2009). Prevalence
estimates of ASD have increased steadily over time from reports of 1 to 5
children per 10,000 in the 1970s. Current numbers from the Centers for Disease
Control and Prevention suggest a prevalence of 114 per 10,000 children (Baio, 2012;
Rice, 2009). It remains to be seen whether there has been a true increase in
prevalence of ASD over time or the reported changes in prevalence can be
explained by changes in diagnostic criteria and increased awareness of the
disorder by parents and professionals. Boys are more likely to be affected with
autism than girls, at a ratio of more than 3:1. About 50% to 70% of children
with ASD also have an intellectual disability.
There is no strong evidence to suggest that individuals with
ASD have a greater risk of hearing loss than the general population. However,
the presence of unusual sensory responses, including abnormal responses to
sound, is considered an associated feature of ASD. For example, individuals with
ASD might completely ignore sounds that would result in a reaction from
typically developing individuals. Other times, they often appear to be overly
sensitive to sound by covering their ears with their hands when loud or
unexpected sounds occur. In addition to these abnormal responses to sound,
young children with ASD are known to lag behind on language milestones.
Therefore, those with ASD will likely be referred to audiologists for hearing
assessments as part of the developmental evaluation to rule out hearing loss as
the cause of language delay. On average, behavioral responses to sound of
children with ASD who have normal hearing are elevated and less reliable
relative to those of typically developing children. Relatively little is known
about higher order auditory abilities of individuals with ASD. However, altered
temporal processing has been recorded in both adults and children with ASD.
Special
Testing Considerations
Children with ASD who have hearing loss are diagnosed, on average,
almost 1 year later than those without hearing loss. Therefore, it is
reasonable for audiologists to be alert to the general behavioral
characteristics of childhood ASD to facilitate referral for evaluation when
indicated. Several screening tools are available that can be used by
audiologists. These include, among others, the Modified Checklist for Autism in
Toddlers (M-CHAT) and the Pervasive Developmental Disorder Screening Test II
(PDDST-II).
Understanding the general behavioral characteristics of those
with ASD can also be helpful to audiologists as they consider modifications to
the traditional test battery. Because the majority of those with ASD exhibit
cognitive deficits, behavioural abnormalities, and hypersensitivity to sensory
stimulation, audiologists should be prepared to address those issues during the
test session. For instance, transitions are often difficult for individuals
with ASD. When possible, audiologists should avoid travel from room to room
with the patient, taking care to escort the patient to the testing area
immediately rather than keeping him or her in the waiting area.
Regardless of the chronologic age of the individuals, audiologists
will need to use behavioral test procedures that are appropriate for their
patient’s cognitive level. This may mean that procedures typically used with
infants and young children such as visual reinforcement audiometry (VRA) or
play audiometric techniques will be used with older children or even adults. If
VRA is used, one should consider minimizing the impact of the reinforcement by
turning off the animation (if a lighted, animated toy is used) or using a video
reinforcement. Other testing options for patients functioning at a
developmental level of 2.5 years or greater are conditioned play audiometry (CPA)
and tangible-reinforcement operant conditioning audiometry (TROCA). TROCA is
often used in pediatric practices that specialize in serving those with multiple
disabilities. TROCA requires the patient to press a bar or a button whenever a
sound is heard, which is paired with the dispensing of a tangible reinforcement
(e.g., small piece of food). TROCA is noted to be particularly effective with
children having cognitive or behavioral (e.g., ASD) disorders. A significant
number of children with ASD receive other clinical services (e.g., speech
therapy).
Patients with ASD are often resistant to earphones or probes
used for individual ear testing. Audiologists can ask the parent or caregiver
to practice listening activities with headphones with the patient prior to the
appointment. If a patient with ASD will not allow the placement of earphones or
probes, audiologists might have to resort to sedated procedures. This is
certainly true if one plans to fit hearing aids. Individuals with ASD are known
to be difficult to sedate with currently available pediatric sedating agents
and are at risk for seizures while under sedation. Therefore, consultation with
the physician in charge of administering and monitoring the sedation process
will need to include notification of the patient’s diagnosis of ASD.

No comments:
Post a Comment