TINNITUS
INTRODUCTION:-
Tinnitus and Hyperacusis are two
challenging in audiology as patients can be desperate and t`here are no cures.
Tinnitus can been defined as a perception of sound (it must be heard,
Involuntary (not produced internationally) and originating in the head (rather
it is not an externally produced sound) , whereas Hyperacusis does not have a widely accepted definition.
Hyperacusis can involve loudness, annoyance, fear and pain. We have noted that
tinnitus is often accompanied by hyperacusis and many current sound therapy protocol
that tinnitus and hyperacusis in parallel.
NEUROPHYSIOLOGICAL CAUSES MECHANISM AND
MODELS:-
Hearing loss can also produce tinnitus. The
most common causes are noise exposure, aging, head injury, and medication. Sometimes
the causes are unknown. The prevalence of tinnitus increase with
Age
and hearing loss, but in particular is influenced by noisy situations report
that the onset of tinnitus is gradual. Initially tinnitus is heard only
occasionally during the day or for brief periods after work. The onset of
tinnitus occurs after the onset of hearing loss. Tinnitus is classified as
either Sensory/neural or middle ear .Middle ear tinnitus is typically related
to middle ear vascular or muscular dysfunction. Sensory neural tinnitus
originated in the cochlea and neural auditory pathway.
AUDITORY HALLUCINATION AS TINNITUS:-
When someone reports hearing sounds that
are like music or voice, it is important to considered mental illness. Reports
of imagined voices or music can occur as part of psychotic illness such as Schizophrenia.
If there is no record of such illness, but there is evidence of depression,
anxiety, or unrealistic thoughts or actions, then these should be addressed
with the client and a referral provided to a mental health professional. In the
absence of indications of mental illness, one could treat this as with other
type of tinnitus. Certainly tinnitus has a central origin. Patients who present
no sign of mental illness and who hear music and voices could benefit from
programs described later. It is important not to overact to the patients
reports.
MEDICAL EVALUATION:-
Often a focus of the evaluation will be
on the cardiovascular system and on metabolic disturbance such as diabetes and hypercholesterolemia.
Laboratory examination (e.g. cholesterol levels, glucose, zinc, and screen for
ototoxic drugs) and imaging tests (e.g. ultrasound, computed tomography scan
magnetic resonance angiography) might be utilized.
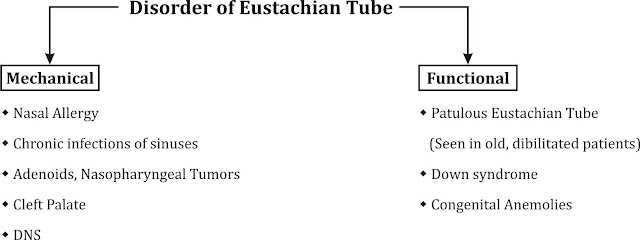
Middle ear tinnitus is associated with
either abnormal middle ear blood flow or middle ear muscle ear muscle
contraction. Some call this “objective” tinnitus” because it can be amplified and
heard by the examiner. Some spontaneous otoacoustic emissions, which are
produced in the cochlea can also be heard. Therefore we prefer the term middle
ear tinnitus. Otologists may determine whether the tinnitus sensation changes
with manipulation of blood flow. These manipulations can change the pulsing sensation.
A proportion of these can be eardrum and can sometimes be observed . Movement
of the eardrum can sometimes be observed visually or with the help of
measurement of air pressure in the external canal with tympanometery. Oral
cavity examination may demonstrate myoclonic activity.
Tinnitus can sometimes be influenced by
movements of the head and neck. Some ototlogists search for sign of
temporomandibular dysfunction which can involve jaw or facial pain or
tenderness and difficulty or discomfort in chewing. Another focus is a search
for treatable sensory neural tinnitus .
Another focus is a search for treatable
sensory/neural tinnitus. This includes some forms of sudden hearing loss, Méniére’s
disease, or a tumor of the auditory nerve. It could be that some forms of
tinnitus might be caused by metabolic diseases and deficiencies (e.g., anemia,
diabetes, hypercholesterolemia, zinc and vitamin deficiency). Evaluations for
these conditions would involve studies of the blood and urine.
Measuring
the Tinnitus
The pitch, loudness, and amount of noise
necessary to mask tinnitus can be measured to quantify tinnitus, provide
assistance for fitting maskers, and monitor changes in tinnitus perception. Patients
can usually compare the pitch produced by a puretone to the “most prominent
pitch” of their tinnitus. Pitch matching can be highly variable, and an indication
of the variability should be reported in the patient chart. Patients can also adjust
the intensity of a tone so that it has the same loudness as their tinnitus.
Sensation level is not a measure of loudness.
The results of a tinnitus loudness match
can be reported in dB sensation level (SL), but this level can only be
interpreted over time for a particular patient if the hearing threshold at that
frequency does not change. An alternative approach is to convert the physical
intensity of the sound into the subjective loudness scale based on sones. Sones
represent an international standard; 1 sone equals the loudness of a 40-dB
sound pressure level (SPL) 1,000 Hz tone (about 49 dB HL) in a normal listener.
A sound that has a loudness of 4 sones is four times as loud. Another measure
of the magnitude of tinnitus is the amount of noise required to mask the
tinnitus, sometimes referred to as the minimum masking level. The noise level
(specify the frequency characteristics of the noise, e.g., broadband 250 to
8,000 Hz) is increased until it just masks the tinnitus. Several things
can contribute to the variability of tinnitus measurements. First, one should
be aware that the test stimuli can change the tinnitus. This is probably more
likely to happen for intense stimuli and when stimuli are presented ipsilaterally
to the tinnitus. The ear receiving the stimuli should be reported. Second, in
many patients the perception of tinnitus is not constant but varies throughout
the day or from day to day. A reasonable approach to this is to make multiple
measurements and report each value. The variability of the measurements can be
documented by replicating the measures and recording the results of each trial
in the patient’s chart. For example, we often use the average of three loudness matches, three minimum masking
levels, and six pitch matches (because pitch tends to be more variable). In patients
with highly variable tinnitus, additional measurements can be made, and the
measurements can be repeated at subsequent visits. Measuring the Reaction to the Tinnitus People’s reaction to their tinnitus covers
a broad range. Some appear not to be particularly bothered by it, whereas for
others, the tinnitus can have a dramatic effect on their lifestyle. The primary impairments can
result in difficulties with thoughts and emotions, hearing, sleep, and
concentration Sleep disturbance is one of the most common of these impairments causing
some to have difficulty falling asleep, whereas others have difficulty falling
back asleep if they wake up in the night. The impact tinnitus is having on an individual’s
life, an easy first step is to ask the person to “list all the problems you
have that you associate with your tinnitus, starting with the problem that
bothers you the most”. This can be done before the first appointment and can lead to an open
discussion of the important problems as perceived by the patient. Several
questionnaires designed to quantify the problems caused by tinnitus are
available. These differ based on the scale used. Our experience is a 0 to 100
scale is easy for patients (a familiar decimal scale like dollars), in which a
patient will respond 0, 5, 10, 15, . . . 100, which enables a 21-point scale. This
provides greater resolution than a 0 to 10 scale. Questionnaires also differ on
the scope of questions asked. Tinnitus
Handicap Questionnaire has been widely used to assess the influence
of drugs, cochlear implants, and sound therapy approaches. Others also include
general questions on the quality of life. We believe this can make the
questionnaire less sensitive to treatment effects, as the quality of life can
be influenced by many factors not directly captured by
treating tinnitus. The Tinnitus Primary Function Questionnaire which focuses on
emotional, hearing, sleep, and concentration difficulties and is sensitive for
clinical trials and assists in determining treatment needs. All appendices can
be found at the end of the book.
TREATMENTS
There are two basic types of tinnitus
treatment strategies: Those designed to reduce or eliminate the physical
perception and those designed to change the patient’s reaction. Counseling
There are various counseling approaches:
They range from providing information to more engaged collaborative counselling.
Many of these are based on the work known
as tinnitus habituation Special
Populations therapy.
Others include strategies for improved coping, management, and behavioral
change. Among these are tinnitus activities treatment, tinnitus retraining
therapy, and tinnitus cognitive behavior therapy . The aim of these procedures
is to provide ways for the person suffering with tinnitus to adjust his or her
reactions to the experience.
The goals of these psychologically based
therapies often overlap. For example, patients can
be helped to habituate to their tinnitus
by de-emphasizing the fear associated with it. Another approach is to decrease the
attention given to the tinnitus, often with the help of background sound. The
way a patient thinks about the tinnitus can influence his or her reactions to
it. Therefore, some clinicians will help patients consider how they think about
their tinnitus. These thoughts can be challenged and revised. Another approach
is to assist patients to change their focus away from their tinnitus. It is our general view that many patients
concerned about tinnitus can adapt to it after the explanation of its origin
and its nonthreatening nature. A substantial number of patients such
reassurance is less effective, and a more elaborate intervention is needed. The
descriptions in the following sections provide guidance on the sorts of
appropriate counseling within the context of general audiologic practice. When
more elaborate counseling is required, reference to the clinical psychologist
is appropriate. Important attributes of the clinician include
• Ability
to listen
• Patience
• Ability
to be encouraging to the patient
• Emotional
insightfulness
• Self-awareness
• Ability
to laugh at the bittersweet aspects of life
• Positive
self-esteem
• Ability
to talk candidly about depression, anxiety, and other psychologic stressors At
the initial interview, it is helpful to determine if patients are curious,
concerned, or distressed about their
tinnitus. Much of the anxiety associated
with tinnitus stems from uncertainty regarding its source and consequences.
Curious patients typically require only basic information regarding possible causes,
mechanisms, prevalence, consequences, and likely outcomes. These patients find
that once the mystery of tinnitus is explained to them, their reaction is
largely resolved.
Concerned patients require more detail and
benefit from information regarding things they can do on their own or other
treatment options. Depending on the level of concern, these patients can
require a more formal evaluation that includes the questionnaires and
psychoacoustical measurements discussed earlier. Distressed patients require
specific tinnitus treatment. Patients with severe anxiety and depression should
obtain help from psychologists or psychiatrists. Patients who report suicidal
thoughts or self-harm need to be further questioned regarding their intentions,
and a referral to clinical psychology or psychiatric services should be made immediately if any concern exists.
PROVIDING
INFORMATION
Most approaches provide information about
hearing, hearing loss, and tinnitus. They usually include the causes,
prevalence, and common consequences of tinnitus. For many people, the unknown
aspects of tinnitus are the most alarming. They often find this basic
information about tinnitus reassuring and may require no further assistance.
THOUGHTS
AND EMOTIONS
It is helpful to distinguish the tinnitus
itself from the person’s reaction to the tinnitus. The way people think and
feel about their tinnitus can have a major influence on their reactions. One
focus of cognitive behavior therapy, and other counselling strategies, is on
challenging a person’s thoughts about tinnitus and thereby facilitating changes
to the reactions to the tinnitus.
MEETING
THE PERSON’S NEEDS
Some counseling procedures go beyond
providing information and attempt to understand and influence the overall emotional
well-being of the patient. Several approaches
are available to help individuals understand and change the emotional
consequences of their experience with
their tinnitus.
COPING/MANAGEMENT
STRATEGIES
Some counseling approaches include
coping/management strategies to help patients understand and change their
perceptions about tinnitus and to modify their reactions and behaviors.
Activities are planned to determine situations in which tinnitus might be a
problem and then to modify their specific situation to reduce these
occurrences. For example, patients might report that their tinnitus is worse
when they first get home from work. This might be a result of sitting in a
quiet room reflecting on the day’s activities. An alternative activity might be
to go for a walk while listening to music, or physical exercise, such as Tai
Chi or yoga, to limber up. Just about any activity that reduces stress can be
helpful.
RELAXATION
AND IMAGERY PROCEDURES
Some patients benefit from learning
specific relaxation or imagery procedures. These can be used when people
experience stress, and it can be helpful for them to learn relaxation strategies
or to focus attention to other thoughts. Exercises to learn how to redirect
attention away from the tinnitus are also employed. For example, in a quiet
room, patients can imagine the sound of waves on a deserted beach. Then, they
can redirect their attention to their tinnitus—then back
to the waves.
Sound
Therapies
Sound therapies include strategies that
use background sounds to reduce the prominence of tinnitus or decrease its loudness
or level of annoyance.
THE
USE OF HEARING AIDS
Most patients with tinnitus also have
hearing loss. Properly fitted hearing aids should help with communication and often
also help with tinnitus by reducing the stress involved with intensive
listening and by amplifying low-level background sounds. Hearing aids are often
the first component of sound therapy for patients with tinnitus.
Tinnitus
Activities Treatment
Our counseling approach has evolved over
the years. We continue to prefer the partial masking strategy we recommended in
the 1980s, although some patients benefit from total masking.
THOUGHTS
AND EMOTIONS
The way patients understand and think
about their tinnitus influences their reactions to it. Providing information in
a collaborative fashion to ensure understanding is essential. Key aspects of
this area include
• Listening to the patient and addressing
issues that are important to him or her
• Providing information about hearing,
hearing loss, tinnitus, and role of conscious and subconscious attention
• Understanding the patient’s reactions to
unexpected, uncontrollable events
• Suggesting changes in behavior and
lifestyle that can facilitate acceptance and habituation
It is important to help patients recognize
the difference between the tinnitus itself and their reaction to it. Cognitive therapy
separates the tinnitus from the patients’ reactions to it and may provide a
sense of control over the impact tinnitus has on their lives.
HEARING
AND COMMUNICATION
Tinnitus and hearing loss often occur
together, but the patients cannot “hear” their hearing loss, so they project their
communication problems on the tinnitus. Reviewing the patient’s hearing loss
and its impact on communication may redirect some of the anxiety to an area
where treatment is more obvious. In addition to hearing aid information, a review
of assertive communication versus passive or aggressive communication styles is
useful.
SLEEP
Understanding normal sleep patterns is the
first step in gaining control over the problem. Other strategies include
• Exploring factors that can affect sleep
(e.g., stress, environmental noise, room temperature)
• Arranging the bedroom to promote sleep
(e.g., comfortable bedding, remove distracting items from room)
• Avoiding alcohol, smoking, and eating before
bedtime
• Using sound to mask tinnitus (e.g., noise
generators or soft radio)
• Learning relaxation exercises (e.g.,
imagery, progressive relaxation)
CONCENTRATION
In our therapy, we discuss the importance
of concentration and things that affect our concentration. We review factors in
the environment (e.g., lighting, background noise, distractions, and
temperature) and personal factors (e.g., being tired, current health status,
and other stressors in our lives) that impact our ability to focus our
attention for a sustained period of time. Activities in “attention diversion” give
patients practice switching attention from one engaging task or stimulus to another. This
type of exercise shows people that they can control what sounds, images, or
other stimuli they consciously focus their attention on. Repeated practice with
this type of activity can help give patients a sense of control over their
attention as well as their tinnitus.